OMG, here we go with more doodles. Ah well...
This post is a summary of the ideas which came out of the Protons thread. I’ve been meaning to write it for some time but the trigger was really Denise Minger’s idea of “carbosis”. This has made me revisit ideas I kicked around at the time of the Potato Diet about the systemic level of insulin and revisited within the Protons concept. I guess the idea is to try and work out whether there is any physiologically plausible explanation for the changes seen under ultra low fat eating, under carbosis.
This is my opinion, most of the references are buried in the Protons thread and some ideas I have interpolated from hard facts because they make sense to me. But be aware you are reading an opinion piece.
Cellular insulin response is controlled by superoxide produced at complex I, which exits the mitochondria as H2O2. Small pulses of H2O2 limit the activity of PTP 1B (protein tyrosine phosphatase 1B). Disabling PTP 1B takes the brakes off of the insulin receptor and allows it to autophosphorylate whenever insulin binds and so allows subsequent insulin signalling to take place.
Large amounts of H2O2 inhibit the autophosphorylation of the insulin receptor directly, at several sites, and so cause insulin resistance per se.
So it's pretty obvious that mitochondrial superoxide/H2O2 controls insulin function and subsequent blood glucose levels, and obesity levels if you are a True Believer, which I am. In this post I'd just like to summarise my own personal thoughts on how the electron transport chain, from where much of the the superoxide is produced, behaves under a variety of conditions.
It is quite easy to set up a mitochondrial preparation which can be driven almost completely through complex I. You can feed it on pyruvate/malate. Under these conditions there is essentially zero H2O2 generation, so there is obviously very limited superoxide generation. Think of it like this:
Electrons from NADH simply drop through complex I, fall easily down hill on to the CoQ couple and are handed on to complex III and the rest of the chain. Similarly we can run tissues on pure glucose at modest levels, even if that's not quite how we do it in real life. Many of Veech's papers on ketones used isolated heart preparations which work quite well for quite some time on oxygenated buffer with glucose alone as the sole metabolic substrate, without insulin. So mitochondria can work on pyruvate and isolated hearts can work on pure glucose.
The next piece of input we need to consider is succinate dehydrogenase (SDH), also known as complex II but I'll use SDH as the term in this post. As the TCA turns using one molecule of acetyl-CoA it generates 3 molecules of NADH and one of FADH2, the later being embedded deep within SDH. The FADH2 of succinate dehydrogenase feeds directly to the CoQ couple and reduces it independently of electrons coming from complex I. We have a situation like this:
The TCA is turning and the ETC is accepting input at two points. This is normal physiology and generates very little superoxide, especially while rest of the ETC is well oxidised and so very willing to accept electrons.
With a mitochondrial preparation it is very easy to supply an input of exogenous succinate to SDH without the rest of the TCA cycling in synchrony. This is an experimental situation, only seen in in-tact animals if they are dosed orally with succinc acid esters. This is what happens:
The diagram doesn't make it terribly clear so lets clarify the flow of electrons from SDH, given a sudden massive rise in isolated succinate. Reverse electron flow to superoxide is picked out in red:
Feeding high levels of succinate to a mitochondrial preparation produces massive levels of superoxide. This is not physiology but it can be viewed as a pharmacological demonstration of physiology pushed beyond its normal limits. It's an illustration.
Aside: mitochondria normally oscillate in their function. The TCA drives complex I via NADH (mostly from the early part of the TCA) to the CoQ couple. SDH reduces the CoQ couple independently so opposes this process. Oxaloacetate at the end of the TCA inhibits SDH, facilitating input at complex I, and the whole system goes back and forth as a normal oscillatory process. That's how it is. I’ve no idea why it’s organised this way, but it clearly works rather well! End aside.
But we can say that some degree of reverse electron flow from SDH through complex I will allow small amounts of superoxide generation which will generate modest pulses of H2O2 as far as PTP 1B. This is essential for insulin signalling.
I feel the next step is to look at the situation where glucose is in oversupply, classically after a pure starch meal. Here we need a brake to be applied to the influx of glucose to the cell. In the aftermath of a glucose based meal we would expect insulin to be high, GLUT4s to be active and ox phos to be based on pyruvate (or lactate if you prefer). What is needed is to reduce insulin signalling, limit GLUT4 translocation and so limit glucose ingress to that which is needed by the cell. This is achieved through a side branch of the glycolytic pathway which generates glycerol-3-phosphate. Among the many, many functions of G-3-P, one is to input electrons from NADH to the electron transport chain from the cytoplasmic side of the inner mitochondrial membrane which will reduce the CoQ couple. How much it does this probably depends on the level of metabolites running down through glycolysis. Let's think about a high glycolytic flux, marked reduction of the CoQ couple and see what happens:
The things to note are a large input of cytoplasmic NADH generating marked reverse electron flow through complex I to generate enough superoxide to send H2O2 to inhibit the action of the insulin/receptor complex. It's a simple negative feedback situation and probably produces quite precise control of access of glucose tailored to the needs of the individual cell. There is no pathology here, it's how glucose based metabolism should be controlled.
The next scenario to consider is something like a large ingress of uncontrollable carbohydrate. A find of honey or table sugar. Let's think about it in the complete absence of any fatty acid metabolism. If we have a sudden avalanche of fructose which pours down through glycolysis, what happens? This unstoppable cascade will activate mtG3Pdh much as the excess glucose we have just considered. This should produce a large amount of H2O2 and disable activity of the insulin receptor and produce enough limitation of GLUT4 translocation to exactly limit glucose access by the correct amount to offset the fructose flood. There are other issues from fructose but these are asides. If metabolism is based on pure glycolysis to supply ox phos substrate then fructose can be accommodated by reducing glucose ingress. From the cellular point of view it all balances out and the degree of insulin resistance is at appropriate physiological levels and only occurs while fructose is high, i.e. not for very long. I'll leave uric acid and metabolic syndrome out from the current discussion, needless to say there are issues, for and against.
So I view mtG3Pdh as a balancing act controlling access of carbohydrate to ox phos by controlling insulin signalling through reverse electron transport through complex I. If these are the only components supplying the ETC it seems to be a pretty simple balancing act which might work rather well. On a pure glucose diet some fructose, even quite a lot, is no problem.
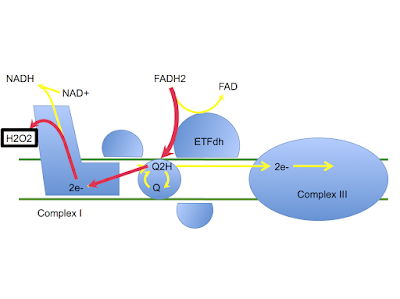
Now we have to add in free fatty acids. While beta oxidation generates acetyl CoA and NADH, one molecule of each for each pair of carbon atoms in the chain, they also generate a molecule of FADH2 at the same time. FADH2 is never used as an unbound molecule, here it is stored within electron transporting flavoprotein which delivers FADH2's electrons to the ETC at electron transporting flavoprotein dehydrogenase (ETFdh in the diagram). Much the same as glycerol-3-phosphate at mtG3Pdh, ETFdh reduces the CoQ couple and is adept at driving reverse electron flow through complex I. Low inputs will do nothing or merely generate small pulses of H2O2 at activating levels, high inputs will generate high levels of H2O2 to shut down insulin signalling on the basis that there is plenty of metabolic substrate from fats, minimal glucose is needed, thank you very much. Again, this is pure physiology, I see no pathology in it.
It looks like this:
The step in beta oxidation which produces the FADH2 to drive ETFdh does not occur when the fatty acid being processed presents a double bond at this step. So fully saturated fatty acids generate the maximum amount of FADH2, monounsaturated fats somewhat less and PUFA least of all. The exception is any fatty acids longer than about 18 carbon atoms, these go to peroxisomes rather than mitochondria. So if we go on to consider monounsaturated FFAs we have something like this:
MUFAs produce significantly less FADH2 so less reduction of the CoQ couple and are not used to generate nearly as much insulin resistance as fully saturated fatty acids. This is not surprising as MUFAs are desaturated versions of fully saturated fats and the desaturation process is largely activated by insulin. MUFAs can be thought of as a more carbohydrate tolerant version of saturated fats.
Of course by the time we get to linoleic acid there is even less FADH2 generated and we have very little ability to resist insulin when these are the main fatty acids being oxidised. Omega 6 PUFA facilitate the action of insulin but don't suppress it even when being metabolised in bulk:
So we can view a glucose system in balance with a fatty acid system where the input to the CoQ couple from the fatty acids controls insulin sensitivity to meter glucose access through manipulating insulin signalling or lack there-of.
Saturated fats suit low glucose availability, MUFA suit a mixed diet and PUFA are spawn of the devil. Near zero fatty acids in the mix rely on mtG3Pdh to regulate glycolysis flux.
I suppose we also ought to think of the situation under a large, uncontrolled fructose input through mtG3Pdh occurring at the same time as saturated fatty acids are being oxidised. That gives us this scenario:
Having two inputs reducing the CoQ couple (as well as a little input from SDH) is a perfect recipe for driving extreme reverse electron transport through complex I with the production of completely unreasonable quantities of superoxide and H2O2. This is the scenario of free radical mediated damage combined with serious insulin resistance. D12079B anyone? The problems are less severe with PUFA fats but this leaves us with a different set of problems, not for today. OK.
Before we go on to look at more human based scenarios using low fat diets I guess we need to consider insulin secretion by the pancreas. This is not solely controlled by glucose. In fact I think I’m going to include the only reference in this post as I don’t think I’ve cited this particular paper before, though I may have done so and forgotten!
Suppress most FFAs using nicotinic acid and you will completely abort the secretion of insulin generated by a glucose level of 12.5mmol/l. Replace the FFAs by infusion and you find that insulin secretion is markedly affected by the nature of the FFAs. The longer the acyl chain the more insulin is secreted. The more double bonds, the less insulin is secreted. At a FFA level around 0.1mmol/l, acutely induced, the pancreas will not secrete insulin in response to 12.5mmol/l of glucose. It seems to me that getting FFAs this low is well within the realms of possibility using a near zero fat diet. You are then in to the region of minimal insulin secretion combined with maximal insulin sensitivity. I know it’s a rat model, a perfused pancreas, assorted artificial lipid infusions, but the logic holds well. Insulin secretion and insulin response/resistance are remarkably similar processes.
So hypo insulinaemia with marked insulin sensitivity might well be the hallmarks of carbosis. I won’t reiterate my thoughts about hepatic insulin extraction except I see this as complementary to the reduced secretion under ultra low fat conditions.
As a True Believer I cannot see steady weight loss without reduced systemic insulin levels. Carbosis suggests that this is the real situation.
The phrase is ITIS, we all know what this stands for. Low enough fat can quite simply cripple the pancreas' ability to secrete insulin in response to glucose. Low enough fat and there is very limited ability to generate superoxide levels beyond normal PTP 1B inhibiting levels. If we accept that hyperinsulinaemia is the driving force of metabolic syndrome and all of its sequelae we have, under conditions of extreme fat restriction, the potential for reducing insulin while using a maximal carbohydrate diet. i.e. There is a health benefit to carbosis, possibly major, implausible as it seems.
There. I said it. You cannot argue with the physiology.
I believe this is what Denise Minger might be describing using "carbosis" as the corollary of ketosis. Under both of these conditions there is minimal insulin secretion but under carbosis there is enough insulin sensitivity working through mtG3Pdh to accurately regulate a near pure glucose metabolism. Fructose is no problem as there is plenty of "exchangeable" glucose for use in a substitution manner. Fatty acids have to be very low for "carbosis" to occur at all and it will be degraded far more easily by saturated fats than by PUFA, as per the ETC diagrams above and as per Denise’s examples.
The essential feature is low insulin. This is the commonality with ketosis. If there are going to be any health benefits of carbosis the low insulin will be the driving force.
So, am I a convert? This is not a religion, what I would ask is:
How effective is carbosis in the real world of T2 diabetes?
As Denise comments:
"More than half of those 100 diabetic ricers—63%—actually saw their fasting blood sugar drop by at least 20 mg/dL during the diet. Only 15% had their blood sugar go up significantly. The remaining 22 saw little to no change".
Translation: Blood glucose: 15% of people were f*cked. 22% it didn’t help. 63% could maintain carbosis.
Insulin usage:
"‘Twas a similar story in Insulin Land. Of the study’s participants, 68 entered the scene already dependent on insulin. As the carbs raged on, 21 of those insulin-injecters didn’t have to change their dosage; nine needed an increase (including four people who initially weren’t on any insulin at all); and—again comes the cruel, cruel defiance of prediction—42 slashed their usage significantly. In fact, 18 folks were able to discontinue their insulin entirely. Feasting on white rice. And sugar. And fruit juice".
Translation: Insulin usage: 13% were f*cked. 29% derived no benefit. 58% achieved carbosis.
How does this stack up against rather mild carbohydrate restriction in severe T2 diabetics?
This diagram says it all. It's from Haimoto et al in 2009.
All they did was drop carbohydrate intake to just over 130g/d. No ketosis. Look at the changes for the first 3 months in HbA1c:
No one needed to increase meds. No one failed to drop HbA1c. No one had to start on insulin. Most people dropped their sulpha drugs. The large spike upwards in the second section looks like one of the two drop outs. The other drop out seems to be lost in the variation in maintenance of control over the 3-6 month interval. Bear in mind that 130g/d is a VERY modest approach to low carbohydrate dieting in severe T2 diabetes. No ketosis, just 100% response rate to a modest carbohydrate reduction.
How can you compare carbosis with ketosis, or even mild carbohydrate restriction? It's like comparing boiled rice followed by boiled rice plus table sugar with a char-grilled fatty steak (rib eye is my preferred choice), buttered broccoli on the side plus Optimal ice-cream to follow. With extra double cream if you're losing too much weight.
The biochemistry of carbosis is very interesting. It might help just over a half of people who try it. Its therapeutic use seems to be of dubious relevance when real food can provide results in 100% of people who comply to carbohydrate reduction. It's strictly for the anhedonic out there but even these poor souls should be cautious about finding themselves in the group of 13-15% who end up f*cked, metabolically speaking.
No thanks.
Peter










109 comments:
Thanks for following up on that.
For those who can't (as in the German attempts at ketotic diet in the presence of cancer) give up their carbs ("I can't give up my bread"), how would one predict which group a particular patient is in? Would empirical testing of response to ELF (Extremely Low Fat) diet be the only way?
Scary.
"The biochemistry of carbosis is very interesting. It might help just over a half of people who try it. Its therapeutic use seems to be of dubious relevance when real food can provide results in 100% of people who comply to carbohydrate reduction."
Low-carb is not 100% effective. At least not for weight loss. Remember Christopher Gardner's weight loss studies?
Low-carb seems quite remarkable for glycemic control in people with type 2 diabetes, but even then, there are some people who swear they do better on a very-low-fat diet (they do seem to be a small minority, though).
From what I understand, someone with a strong family history of type 2 diabetes and/or very high triglycerides should try a low-carb diet first. What would be the markers for those who would do better on a very-low-fat diet? And what about those people who don't get anything magic happening on either diet?
Damn it PETER! ... I guess I have another experiment to do. :)
Brilliant as usual Peter - and in the nick of time - I was just about to insinkerate my rare duck breasts and tuck into a sh"tty bowl of rice... :-)
Thank you, Peter, much appreciated. :-)
Fascinating ideas! Thanks for adding your voice to the 'carbosis' discussion -- I do think there's much to be learned here.
"Its therapeutic use seems to be of dubious relevance when real food can provide results in 100% of people who comply to carbohydrate reduction."
As I understand it, results from carbohydrate reduction (independent of weight loss) are more of a lifelong band-aid -- working only as long as carbohydrates remain minimized -- whereas 'carbosis' has the potential to actually restore normal glucose tolerance in some individuals and allow for a more flexible diet over time. I think that makes the superiority of LCHF less clear-cut, if the low-fat route might have the potential for something resembling an actual cure for diabetes. The key is identifying the individuals who might respond in such a favorable way and using LCHF for those who wouldn't.
Thanks for the biochemistry lesson again Peter. It sounds like some can get by on high carb if they eat very little. It's just that more will do better on high fat and also eating less.
So, according to Denise's logic, you could eat HCLF until your normal glucose tolerance is restored, and then revert to LCHF permanently? Is there a case to be made for oscillating between the two extremes, and if so, what would be the minimum time periods for each? I'm guessing there would be little point to doing this, given the time frames for full ketoadaptation. Additionally, is one form of eating more preferable for weightlifters?
Crap! And my honey-lemon rice on a bed of figs and molasses was almost ready. :(
Hi all,
I have to say that I do not have my clinician’s hat on. I developed an idea about what, underneath deep layers of metabolic signalling processes, might be the basic features of nutrient processing at the most molecular level. I would never have predicted the carbosis effect but, once presented with it, I have to believe the data and try see how it fits in with my concept. That’s very ad hoc-ish and it’s a big leap to start making predictions.
For people who appear unable to give up sugar I think we have to be very careful to try to tease out societal conditioning vs metabolic responsiveness. @annlee: Do people who avoid fat do so because they are victims of conditioning to avoid fat or do they get fat because they feel better when they eat sugar? I don’t know. What would help for the cancer patients who couldn’t stop eating sweets is hard to predict and certainly modern attempts to use the Gerson Therapy have not been impressive, there is one at lest one report in pubmed.
@valerie: Yes, I’ve considered Christopher Gardner twice and he fits with this post. He can achieve carbosis. At least 50-60% of people can probably do the same. What is cultural and what is biochemical about people who can’t manage it is interesting. We know from the coastal inuit that there is positive selection pressure under some circumstances for a mutation which has limited ketosis ability. Are there other selected responses which limit ability to achieve carbosis vs ketosis? There are deep layers of control interposed between whole body and electron transport chain. “We are not broken” is a phrase I find as difficult to accept as the idea that evolution stopped 10.000 years ago. It accelerated. We all “break” eventually, oddly enough.
@Steve, you are probably aware that I don’t think LCHF ever cures anyone of the underlying defect of complex I that we label as T2 diabetes. Side steps it, yes, very effectively. But can you go back to living on pizza and Fanta and expect to maintain health. This is what I would call a cure. “Cure” is a four letter word beginning with c…
@Denise, I absolutely do not expect LCHF to be a cure. Although there are people out there who would disagree with that expectation. So far the modern published data on ultra low fat suggest it works for 3-6 months. Barnard learned very well that you only ever report at 22 weeks. Whether this is social or metabolic remains to be seen. He got his fingers burnt publishing his 74 week study and his publications since have feature a time frame limited to the initial improvement period. I’m waiting for the carbosis equivalent to Nielsen and Joensson’s 176 week publication, where a small number of LCers stuck to it for years with an average HbA1c lower that that of the Barnard group’s nadir at 22 weeks. If carbosis can do this, fine, it allows another arrow in the quiver. Personally I don’t see it coming but I stand ready to be corrected. Perhaps there are long term carbosis datasets from over the last few years about to be published tomorrow. We’ll see. All we need is replication under modern conditions.
LC works for life, it’s not so arduous. Carbosis reminds me of chemotherapy, people look forwards to it being over!
@jeff, I don’t think we have answers here. Both approaches limit appetite. Which do best long term?????
@Dissertante I’m not sure reversion to LCHF would be the plan. My own biases stop me considering leaving LCHF in the first place. Steve will find out for us #;-)
Peter
Very interesting discussion. I'm reminded of Kwasniewski's claim that a very low fat diet, which he calls the "Japanese diet", is the second best diet, after his Optimal Nutrition. But he hastens to add that with time many people develop problems on the Japanese diet. In any case, it is mixed eating of carbs and fats that does the greatest damage.
What about metabolically healthy people eating LFHC? Kitvans, perhaps. Does the very interesting carbosis concept fit with the potential long term healthfulness of this?
From a LCHF perspective I've always been bothered by the "paradox" of the seemingly quite healthy, well-studied high carb populations. It's a huge data point, hard to close one's eyes to. Even if LFHC might not be an optimal default diet for the metabolically broken, could it be a healthful traditional diet that, if followed continuously, never leads to the brokenness in the first place?
WilliamS,
The Highland Bantu in Tanzania run at about 7% fat and 82% carbs, they're vegetarians and have a progressive rise in BP with age. Their intermarriage-mingled equivalent Bantu on the lakeside eat fish as well as rice and corn so run at 12% fat. They have no equivalent BP pathology. 7% fat of vegetarian origin suggest the Highland Bantu are in carbosis, with worse CV health than those related Bantu eating half a kilo of fish a day.
Peter
Thanks for the doodles Peter, they are much appreciated.
One day they will be carved into coloured blocks for pre-schoolers to assemble in their basic metabolism classes.
@denise,
some thoughts on clinical applicability and confounders
I have no doubt the guy in Fat Sick and Almost Dead reversed whatever it was he had on his juicing binge. I have always thought, for as long as I have cared, that there is more than one way to skin the metabolic cat.
However - what about the gradations leading up to carbosis or ketosis? It seems pretty clear that a diet of 30% CHO outdoes a diet of 30% FAT if isocaloric or ad lib. Kirk et al 2008 show that reductions in HbA1c, FPG and TGs are proportionate to degree of CHO restriction from quite high in the scale.
Do we have any comparative data on the approaches to carbosis?
Further, Esseltine and the rest, including the vegetarian Bantu, do not, so far as I know, drench their food in sugar, honey or rice syrup the way low carbers drench theirs in butter, coconut oil, and olive oil.
Their plant-based diet is high in fibre, and the fermentation of fibre produces butyrate. The amounts of butyrate (and acetate and propionate) generated may not be so great as to tip the CHO-FAT balance backwards very far, but nor are ketone levels that high in ketosis - and butyrate etc are the country cousin of the ketone bodies, with easy access to the TCA and effects on AMPK that carbs alone could not produce.
Thus butyrate, by reducing hepatic fat (and FAIK pancreatic fat) independently of macros, increases insulin sensitivity and lowers BG. Which is something that can potentially apply to a low carb diet too with all those non-starchy veges, but may be favoured in a low-fat gut.
http://www.ncbi.nlm.nih.gov/pubmed/23696823
New term, but carbosis is as old as Kempner circa 1950 and the now-defunct rice diet.
http://hyper.ahajournals.org/content/64/4/684.full?sid=a02c30c9-7dcf-4cc9-ad9a-d5e2cbf7be6c
Who and What Drove Walter Kempner?
The Rice Diet Revisited
an excerpt:
The 49-year-old diabetic hypertensive patient was admitted to Duke University Hospital because of shortness of breath. His family members had died mostly of myocardial infarction and stroke. Renal failure was also in the family history, albeit irrelevant because there was no treatment then available. The patient had been overweight all his life. The admitting blood pressure was 200/130 mm Hg. Examination disclosed papilledema and malignant hypertensive eye ground changes bilaterally. The neck veins were distended, and the breath sounds were diminished bilaterally in an area where dullness was increased; above the lung bases, rales were audible. A third heart sound was apparent. The liver was enlarged, and copious (4+) peripheral edema was evident. The protein excretion was >1.5 g per day. Phenothalein excretion after intravenous injection was diminished. The nonprotein nitrogen concentration was increased; the hematocrit was decreased as were the plasma proteins.
Previous Section
Next Section
What Is to be Done With Such a Patient (in 1939–1949 or Later)?
Kempner, on the basis of his earlier cell metabolic studies and experiences in German departments of internal medicine, adapted a regimen to comply with the medical students’ challenge. The diet he designed consisted almost entirely of rice and fruit. The diet provided ≈2000 calories per day. Kempner occasionally reluctantly permitted addition of breads or treats. In essence, the diet comprised 4% to 5% protein (<20 g per day), 2% to 3% fat, and the rest was complex carbohydrates. The sodium content was 150 mg (<10 mmol/d). Fluid intake per day was restricted. Kempner was aware that white rice might be thiamine deficient and included a vitamin preparation. He also included citrate-containing fruit juices with the idea that any metabolic acidosis could be counteracted that way. If we compare that regimen with the US diet of then (and now), we observe 25% protein, 25% fat, and 50% carbohydrates. Furthermore, the daily salt intake would entail ≈9 g (Na+ and Cl−, 150–160 mmol). Thus, the Kempner diet was (dramatically) low in salt (Na+, ≈10 mmol/d), low in protein (<20 g/d), low in fat, and high in complex carbohydrates. Kempner was interested in winning the clinical battle, less in which constituent (salt, calories, protein, carbohydrates, or fats) was the most important regarding any particular separate effects. Results from this patient are shown in Figure 1. Sorry, couldn't get a link to come across. In the paper, though.
Peter, could it be that both Bantu populations are basically in Denise's carbosis, and that the vegetarians' health suffers somewhat because . . . they're vegetarians? Fish is healthy (according to the proprietors of our beloved local sushi joint, at least).
Perhaps I'm mistaken, but I thought a number of well-studied populations, e.g. Kitavans, have been shown to be metabolically very healthy, with an absence of the diseases of civilization, on their traditional low fat, high carb diets. If this is not the case then OK. But if it is, it requires explanation. I was just wondering if Denise may have hit upon one that might just work.
Nice discussion, Peter.
Denise has written a very interesting post, but seems a little over-enthusiastic considering the discussed studies' possible lacks of:
- an independant analysis of the raw data;
- ditto for the experimental designs;
- caveats such as the obvious conflict of interest between the (e.g.) Pritikin Longevity Center's wish to attract a clientele and doing its own studies;
- duplication of the studies by other researchers.
I realize that these niggling points are the standard ones, but that's because the associated flaws are so ubiquitous in the medical literature (begin rant) (the only field that can provide seemingly endless amounts of publish-or-perish grist from some experiment that was done decades previously and was problematic to begin with.) (end rant)
Regardless, Denise is to be commended for her energy and bringing those old studies to light.
Missing from this thread -
1 - My take is these diets also tend to be low in protein and I expect that besides losing fat weight they lose muscle - not so good based on the correlation with survival.
2- Losing weight is a 'good thing'^tm but what if the long term effects of a BG drifting up causes an increase in cancer and the other age accelerating effects of elevated BG? (I think likely).
3- Quality of life? Many fad diets work - as long as you don't mind being hungry. A friend of mine is on the 'potato diet' - allowed to eat what he wants once a week. Says he feels better that day. There was the Austrian study that showed a correlation with vegan diets and mental problems and more: Nutrition and Health – The Association between Eating Behavior and Various Health Parameters: A Matched Sample Study
http://www.plosone.org/article/fetchObject.action?uri=info:doi/10.1371/journal.pone.0088278&representation=PDF
Also - might screw up your love life -
http://www.telegraph.co.uk/men/active/mens-health/11172519/Vegetarians-have-much-lower-sperm-counts.html
Hi Peter,
Thanks for the response!
If you're referring to the study by Neal Barnard (not RJ Barnard, who did many of the Pritikin studies), the vegan group's fat intake was 22.3% at the end of the study (see http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677007/table/tbl2/). It either did not hit the "magic" zone, or did briefly (up until 22 weeks?) and then rebounded. So, I'm not sure we can conclude much about long-term carbosis from a diet that didn't actually maintain a carbosis-level fat intake.
Interestingly, the follow-ups (up to 5 years) for the non-vegan Pritikin Program were much more promising for diabetics, and for MS, the results of the non-vegan Swank program were more promising than the vegan McDougall version. I suspect -- but can't yet prove -- that a strict vegan version of carbosis is detrimental in comparison to a non-vegan version, which at least provides a higher protein intake and a higher (though still low) level of fat-soluble vitamins, among other nutrients. Given the Pritikin and Swank studies were less rigorous in terms of control groups and design, that can only be speculation for now, but it does make me wonder if the commingling of animal rights' activism and whatever therapeutic effect is present in 'carbosis' has been a detriment to the low-fat community.
BTW, in Nielsen and Joensson's 176 week study, 8.5% of the low-carb group suffered cardiovascular events, possibly 13% if the sudden death was from atherosclerosis. In Esselstyn's 192-week study of heart disease patients (http://dresselstyn.com/JFP_06307_Article1.pdf), only 0.02% of adherent patients experienced heart disease progression. The N&J study would need a much bigger sample size for us to really draw comparisons, but looking at other forms of morbidity and mortality from low-fat vs. low-carb is also worthwhile.
Oh my -- that should be 2% for heart disease progression in the Esselstyn study, or 0.6% for actual cardiovascular events related to disease recurrence (one stroke).
Hi BP,
I agree with the concerns you express about the studies. I'd probably be much more ruthless with them if not for the mechanistic studies supporting and explaining their results, which will be Part 2 of the blog post. :)
@ Denise,
surely you're aware that Nielsen and Joensson included a control group on the normal diabetes diet and that the CVD death rate in this group was much higher than in the larger low carb intervention group - even though the control group was halved and the treatment group increased by half at the 6 month point?
The control diet - Proportions of carbohydrates, fat and protein for this group were 55–60%, 25–30% and 15% respectively. In the normal diabetes diet whole-grain products are recommended. Generous helpings of vegetables and several servings of fruits as snacks between meals are also recommended.
One stroke case, one heart failure case, and one death among the low carb group of (at 6 months) 23 (which included at least 2 drop-outs by the end), plus another 3 cases who switched from control diet after the 6 month period (total 26).
4 MI cases, two of whom died, among the 5 controls left by the end.
This is comparing apples with apples - it tells us that Nielsen and Joensson were treating a high-risk population.
Weight at baseline average was 100Kg
BMI was 36.1
HbA1c 8%
6 patients used statins
Age, gender mix, smoking, isn't recorded in the papers I have.
Weight in Esselstyn's study isn't recorded, there is understandable weight loss, but I suspect if weight or BMI had been a major issue it would have been in the baseline data.
Hi George,
Indeed, Nielsen and Joensson were treating a high-risk population. So was Esselstyn -- everyone in his group already had established coronary artery disease!
Of the non-adherent patients in Esselstyn's study (who failed to avoid added oils, dairy, and meat), 13 out of 21 (62%) experienced adverse cardiovascular outcomes: 2 cardiac deaths, 2 strokes, 4 PCIs with stents, 3 CABGs, 1 endarterectomy for PAD, and 1 heart transplant. Of the adherent patients who stuck to the prescribed diet, only 5 out of 177 (3%) experienced adverse cardiovascular outcomes related to the nutrition intervention: 1 stroke, 2 CABGs, 1 restenting.
Esselstyn's diet: "The core diet included whole grains, legumes, lentils, other vegetables, and fruit, and avoidance of all oils, fish, meats, dairy products, avocado, nuts, sugary foods, and excess salt."
If weight or BMI hadn't been a major issue, I consider that a strength of the study, as that means the results aren't confounded by significant weight loss from an obese baseline (possibly a problem with the N&J study?).
Thanks, Peter. Very interesting discussion.
Does anyone know if there any biochemical analysis by the proponents of VLF that are similar to Peter's?
And how does extreme calorie restriction with low-fat plant-based diet, such as the New Castle diet, fit in?
Finally does anyone see how this applies to the epidemic of metabolic diseases that we see today? At best it looks like VLF may be a short-term therapy. Personally I still favor the carbohydrate-insulin hypothesis put forward by Taubes and others.
@ Denise,
good points.
I have an explanation for the success of the rice diet etc which is, that when lipids in the diet (fats and cholesterol) are seriously restricted, DNL cannot supply enough fat and cholesterol for fuel and function, and therefore scavenging and recycling of lipids goes on.
Whereas the success of ketogenic diets is due to the pathway to further synthesis and accumulation of lipids being shut down, with the same result.
Lipids accumulating in pancreas and liver and muscles reduce insulin sensitivity, so either way this is restored.
Absolutely agree. I use the phrase, "successfully self-treat". :)
<<@Steve, you are probably aware that I don’t think LCHF ever cures anyone of the underlying defect of complex I that we label as T2 diabetes. Side steps it, yes, very effectively. But can you go back to living on pizza and Fanta and expect to maintain health. This is what I would call a cure. “Cure” is a four letter word beginning with c…>>
I don't know if diabetes is ever reversed. When I look at the bariatric surgery research I see diabetics becoming pre-diabetic and on a very restrictive diet low in carbs/fat and high in protein. Hardly a reversal or cure and this is the gold standard for diabetes reversal.
I think Type II diabetes can be ameliorated (as George H mentions - by reducing the ectopic fat build-up by in the pancreas, liver and I'd also add by resistance training improving muscle sensitivity) and managed by better diet.
But I seriously doubt anyone is going back to Pizza / Coke once their Type II has progressed.
Peter, what time scale(s) do you suppose the superoxide mediated regulation of insulin sensitivity operates at? Is it strictly very short term, within-meal, thus responding only to the macronutrient content of the current meal? Or is is regulated over longer time periods so one responds very differently to a high carb meal, or to saturated fats, or what have you, if one has been eating a ketogenic diet for a few weeks vs. say a carbolic diet?
Hi Denise, yes, I think I do have the wrong Barnard, mea culpa!
OldTech, as far as I’m concerned the Newcastle diet was a near complete failure, can’t recall the numbers but few maintained their improvement and the starvation sounded appalling.
Other generally points that might be salient. Carbosis protocols appear to limit protein. Within reason this strikes me as a good thing. If you really can lower insulin and mTOR activation at the same time the people who do respond might do well.
Two of my biggest concerns about my own approach of LC in general is the probability of omega 6 PUFA creep which I think will mess up the ETC in many ways, and protein creep which will activate mTOR and may promote ageing better than insulin itself (probably) does.
While clearly I still fall in to the LC camp the carbosis state (without the name) has been interesting for some time, not anything I would consider trying of course. But it strikes me as a potentially very high risk approach if compared to my longer term low grade concerns about “drifted” LCHF eating…
Peter
WilliamS, both. I think it will be tonically elevated during fasting on fats and acutely in response to meals depending on what was eaten. I'm also curious as to whether all superoxide/H2O2 is the same. Does some get specifically channelled to the insulin receptor? Is the insulin receptor physically associated with complex I for direct hand over? Does cytoplasmically generated H2O2 interact with complex I derived H2O2 for insulin signalling? Lots of questions.
Peter
I have followed you for a year or so now! Don't you dare even consider doing that to your body or health! :)
Not to hijack the thread, but worthy of note. Peter called it on the next CETP inhibitor to fail. Eli Lilly gave up on evacetrapib today.
http://www.medscape.com/viewarticle/852516
I had a musician friend who lived on nothing but potatoes when times were hard. And then his hair started to fall out. I didn't hear what happened to his teeth.
So it might be also interesting to see what happens when you tip the macro-nutrient scales over to protein and nothing else. HPLCLF. The words Rabbit Starvation spring to mind but maybe that is just from doing high protein 'badly'?.
Apparenetly those sufferering from rabbit starvation will eat any fat they can get their hands on ... or even carbohydrate.
C.
Nice find Bob. Not completely surprising. On to the Peskies next...
Peter
@Passthecream - supposedly the Protein sparing modified fast used "high quality" protein (skinless chicken breast, tuna, cottage cheese (?!), egg whites) to spare muscle breakdown and allow the unimpeded burning of fat. It was supposed to be a *temporary* hack for the morbidly obese. But it seems the muscle breakdown during fasting has been wildly exaggerated. The most accessible write up I've seen so far is the latest from Dr. Fung.
Even if we consider very low fat diets to be a good alternative way to keep our body fat from wrong places like liver and pancreas (for thous who can be not super-hungry while eating little amounts of fat), what about fat-soluble vitamins and vitamin A which can be found only in animal products? I am sure Denis met more vegetarians than me, and some of them may be thriving, but I yet to see one who is thriving on plants. There are a several of vegetarians in my yoga circles, and I observe the same people for longer than 10 years. My impression is that younger people can look and function good even on a deficient diet, among my son's rock-climbing friends some vegetarians, but it starts to show more as people age.
Re: protein
Sometimes I wish I'd never read Rosedale. Limiting protein to his levels (~1g/kg) while sharply limiting carbohydrate requires lots and lots of added fat. Pleasant of course when you can do it, but sometimes a real challenge, e.g. eating out, and not easily compatible with some of the world's great cuisines. This highly restricted way of eating can come to seem like hard work rather than enjoying Food.
Rosedale makes sense mechanistically, but so often the world doesn't obey our clever models when you actually make the necessary observations. Is there believable evidence in real human populations that protein > 1g/kg ages and sickens us?
+1 What William says and asks, Rosedale's protein limitations always stick in my head and I would like to know also if there is recent believable evidence with regard to higher protein intakes.
I'm also interested in knowing whether higher protein intakes for recreational weight lifters are damaging.
Perhaps a minor point, but the low-fat approach clearly isn't necessarily for the anhedonic (those with the inability to feel pleasure). Research indicates that we undergo hedonic shifts corresponding with our diets. In other words, low-fat eaters experience a shift in cravings away from fat.
"Hedonic (ie, pleasantness) ratings for high-fat foods and preferred fat content of selected foods declined, but only in the group deprived of sensory exposure to fats. Thus, the frequency of sensory exposure to fats exerts a stronger influence on hedonic ratings of foods containing fat than total fat intake. The hedonic shift may promote long-term compliance with a reduced-fat diet."
— http://www.ncbi.nlm.nih.gov/pubmed/8438771
More recent research shows that this same hedonic shift occurs in low-carb dieters, whose preferences eventually shift away from high-carb foods. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3139783/
Anecdotally, not only do I no longer crave high-fat foods, but the mouth-feel of grease / oil has become unpleasant. So, in my case, it's not just a lack of craving, but an active dislike of some high-fat foods.
Again, this is perhaps a minor point, but I thought I'd throw in the perspective of one who is deriving much pleasure from consuming a whole-food, omnivorous diet that happens to be low in fat (10-15%).
Anecdotal evidences are not uniform . When Cholecystitis at first (diagnosed at age 10), than gall-stones, and at last a removal of my gall bladder provided a good adherence to a low-fat food in my case, it didn't cause me to dislike fat, rather to be very cautious of it. I used to be hungry almost all the time. It took me more than couple years to train my body to be fat-friendly. I eat a diet high in fat and low in carbohydrates now. BTW, whole foods does't equal to low-fat foods.
It is often the case that people gain weight after their gallbladder is removed. I suspect it happens because everything fatty is causing an immediate diarrhea, and many give up on eating fat.
Peter, you referred to that Stein et al paper before, and made insightful comments but I have lost track of them again, temporarily.
You referred to this paper in 2008
http://www.ncbi.nlm.nih.gov/pubmed/15579777?ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
where the crossover carb levels were certainly in carbosis territory
and you wrote:
'we see that there was essentially no difference in fasting free fatty acids, yet the fasting triglycerides in the high fat period were half those of the high carb period. we see that there was essentially no difference in fasting free fatty acids, yet the fasting triglycerides in the high fat period were half those of the high carb period. '
C.
ah double paste there, sorry.
Also damned if I will be changing my pen name to Pass The Potato. 2000cals of sweet potato/day - that's about 2.5Kg I think. My goodness the gas levels ... global warming ...
C.
To say that LCHF diet does not cure T2D, is irrelevant. Does vitamin C cure scurvy? Does eating cure hunger? If you have a condition which can be reversed and brought back to normality, it just means that you should not go looking for trouble. Antibiotics cure infections, but you will still get more infections if you repeat whatever it was which gave you the infection in the first place.
I wonder if there's an ETC explanation for this:
https://www.dropbox.com/s/2f3fbj7pzxnn6ye/Lauric%20acid%20colon%20cancer.pdf?dl=0
Induction of apoptosis by the medium-chain length fatty acid lauric acid in colon cancer cells due to induction of oxidative stress.
In Caco-2 cells, lauric acid reduced GSH availability and generated ROS compared to butyrate (p < 0.05). Lauric acid reduced Caco-2 and IEC-6 cells in G0/G1and arrested cells in the S and G2/M phases. Lauric acid induced apoptosis in IEC-6 cells compared to butyrate (p < 0.05). Butyrate protected IEC-6 cells from ROS-induced damage, whereas lauric acid induced high levels of ROS compared to butyrate.
George, in the materials, 'Sodium lauric acid' --- is that the soap?
C.
John U said -
"To say that LCHF diet does not cure T2D, is irrelevant. Does vitamin C cure scurvy? Does eating cure hunger? If you have a condition which can be reversed and brought back to normality"
Hi John.
It's not necessarily so cut and dried as that I believe John. I get what you are saying but Scurvy is a disease caused by Vitamin C deficiency, but the proof isn't there that lots of carbs per se cause TD2.
Cutting back on the carbs for a T2 diabetic is definitely a good thing to manage the disease but cutting back may also stress other parts of the body over the long term - such as the thyroid and digestive systems. And I say may. I certainly don't know, but many people do report problems over the long term when they restrict carbs too much.
What actually causes TD2 though? It makes sense to look at avenues including such things as a lack of nutrients (as not found in empty carbs of course).
I'm definitely far from any expert, but I do take stock in the idea that many healthy people and cultures have included a fair degree of carbs in their diet and remained (and remain healthy).
Michael44 thinks that it makes sense to probably eating too much simple carbs may cause TD2 due to lack of nutrients. However, the famous rice diet consisted mainly of white rice, sugar, fruit, fruit juices.
Michael
" the proof isn't there that lots of carbs per se cause TD2. "
I think that what Peter is explaining here is that there is more than one pathway to the disease and also to the 'cure' and both are intimately tied into energy and insulin dynamics. The animal cell being a very complex device, it is replete with fail-safes and alternatives and damage control mechanisms. Problems occur when the fail-safes fail. It is probably a mistake to think of type 2 diabetes as just one thing and apparently in the low-fat lit that Denise is recounting it looks like it might also be a mistake to call insulin dependent type 1 diabetes a single monolithic thing. Complex, complex complex.
But to simplify, it seems that T2D is broadly caused by eating too much of anything and everything in the same way that Pate de Foie Gras is caused.
C.
Hi Galina.
"Michael44 thinks that it makes sense to probably eating too much simple carbs may cause TD2 due to lack of nutrients. However, the famous rice diet consisted mainly of white rice, sugar, fruit, fruit juices."
As one possible cause Galina, yes. I believe nutrients should be investigated more than they have been in my book (as one possible cause of our chronic diseases such as T2D). I think there has been too much emphasis placed in the past few years on the extreme limiting of carbs as being the best way to achieve good health (keep in mind that I am definitely not saying that people should'nt go high-fat, if that's what works for them).
Regarding the Dr Kempner diet, if it cures some people's diabetes, then good-luck to them. I'm all for what works, but I agree with Passthecream that the disease may be multi-faceted and multi-causational. I'm guessing that you're not suddenly going to go out and try the diet, are you? - even though Dr John McDougall has this to say about it -
"Although low-tech, the benefits of the Rice Diet far exceed those of any drug or surgery ever prescribed for chronic conditions, including coronary artery disease, heart and kidney failure, hypertension, diabetes, arthritis, and obesity."
Sure, the disease of TD2 is multi-faceted and multi-causational because it is just one of many possible manifestations of malfunction of a complex body system. May be in order to keep a realistic point of view on a human health, it is useful to remind yourself about lows of complex systems from time to time. He re is a good example of reading "How complex systems fail" http://web.mit.edu/2.75/resources/random/How%20Complex%20Systems%20Fail.pdf.
It is hard to choose, but I just want to bring that long citation
"6) Catastrophe is always just around the corner.
Complex systems possess potential for catastrophic failure. Human practitioners are
nearly always in close physical and temporal proximity to these potential failures –
disaster can occur at any time and in nearly any place. The potential for catastrophic
outcome is a hallmark of complex systems. It is impossible to eliminate the potential for
such catastrophic failure; the potential for such failure is always present by the system’s
own nature.
7) Post-accident attribution accident to a ‘root cause’ is fundamentally wrong.
Because overt failure requires multiple faults, there is no isolated ‘cause’ of an accident.
There are multiple contributors to accidents. Each of these is necessary insufficient in
itself to create an accident. Only jointly are these causes sufficient to create an accident.
Indeed, it is the linking of these causes together that creates the circumstances required
for the accident. Thus, no isolation of the ‘root cause’ of an accident is possible. The
evaluations based on such reasoning as ‘root cause’ do not reflect a technical
understanding of the nature of failure but rather the social, cultural need to blame
specific, localized forces or events for outcomes...
8) Hindsight biases post-accident assessments of human performance.
Knowledge of the outcome makes it seem that events leading to the outcome should have
appeared more salient to practitioners at the time than was actually the case. This means
that ex post facto accident analysis of human performance is inaccurate. The outcome
knowledge poisons the ability of after-accident observers to recreate the view of
practitioners before the accident of those same factors. It seems that practitioners “should
have known” that the factors would “inevitably” lead to an accident.2 Hindsight bias
remains the primary obstacle to accident investigation, especially when expert human performance
is involved."
As a naturally unskilled human operator of my own complex body system, I could report that I lived on a very low-fat diet before and after a gallbladder surgery, and it didn't improve my health a little bit, even though before the surgery I lost some fat because almost any food could cause colics. No, I am not about to try a rice diet, and fortunately, now I have no reasons to do it. My body system works better now on LC. I used something similar to the official rice diet (unsalted cooked rice and a sugar-free compote made out of dried apricots and prunes) in my early youth as a crash 3 days slimming regiment in order to fit better in some garments. It is a very hard to stay on a such diet, which is a bid negative.
May be it is sad to think about it, but we live to fail eventually.
Let's look at this as if
a) benefits of fat restriction are proportionately equal to those of carb restriction
b) we want to roll this out to help people
Despite scientific consensus in favour of fat restriction for decades, therapeutic fat restriction was only achieved in a few largely self-selected populations mainly under medical care of exceptionally charismatic gurus. Because it is hard.
Despite scientific consensus against carbohydrate restriction, therapeutic carbohydrate restriction has been achieved by a) self selected free living humans, and b) the majority of randomly selected subjects in diet trials conducted by only slightly extraordinary medicos.
Because it is a hell of a lot easier.
So where should we put our health dollars and our effort as a policy of first resort?
George, I used to agree with you that LF is hard. I've never tried it, but it seems like too many people claim that they do it easily. They can't all be hypnotized by a charismatic leader. Denise, for example, is eating LF and loves it. She tried LC and still prefers LF for health and happiness.
Perhaps it's genetics? Perhaps it's just adaptation? IDK.
Somebody posted this comment on Denise's blog:
"Perhaps a minor point, but the low-fat approach clearly isn't necessarily for the anhedonic (those with the inability to feel pleasure). Research indicates that we undergo hedonic shifts corresponding with our diets. In other words, low-fat eaters experience a shift in cravings away from fat.
"Hedonic (ie, pleasantness) ratings for high-fat foods and preferred fat content of selected foods declined, but only in the group deprived of sensory exposure to fats. Thus, the frequency of sensory exposure to fats exerts a stronger influence on hedonic ratings of foods containing fat than total fat intake. The hedonic shift may promote long-term compliance with a reduced-fat diet."
— http://www.ncbi.nlm.nih.gov/pubmed/8438771
More recent research shows that this same hedonic shift occurs in low-carb dieters, whose preferences eventually shift away from high-carb foods. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3139783/
Anecdotally, not only do I no longer crave high-fat foods, but the mouth-feel of grease / oil has become unpleasant. So, in my case, it's not just a lack of craving, but an active dislike of some high-fat foods.
Again, this is perhaps a minor point, but I thought I'd throw in the perspective of one who is deriving much pleasure from consuming a whole-food, omnivorous diet that happens to be low in fat (10-15%)."
Michael44 said: "...the proof isn't there that lots of carbs per se cause TD2."
But the proof IS there that lots of carbs
per se cause the symptoms of T2D.
bill said - "But the proof IS there that lots of carbs
per se cause the symptoms of T2D.
I made a mistake there bill - my sentence should have read "...per se whole-food carbs".
I am definitely not advocating isolated carbs as a long term solution to anything, although the Dr kempton diet is food for thought for anyone struggling (for short-term benefit maybe - i.e I haven't read this post of Peter's, nor Denise's recent post yet, but I'm guessing the Dr Kempton diet is meant to be for short term use, not long-term?).
Having said that bill, I am not a diagnosed diabetic and if I drink a can of coca-cola I'm guessing that my "symptoms of T2D" will not be nearly as apparent as someone who is actually T2D. I mean, if someone has renal disease and has to go onto a protein-restricted diet because they can no longer adequately get rid of their nitrogen waste, we don't automatically blame protein as being the cause of the kidney disease. Or, at least we shouldn't, should we?
Galina, what you have said and presented seems fair to me, and that's why it's good to read that some people in the high-fat arena are looking at diabetes from a position that involves a lot more than just touting the advice that it's been the carbs that are killing us. And I'll bring you in here as well George, I just don't think there has been enough distinction within the high-fat community between carbohydrate foods - there's been way too much emphasis on cutting all carbs rather that carbs from specific foods. All carb foods ain't equal is my point.
I just want to reiterate that I am not anti-fat. Far, far from it. But the high fat diet does end up causing problems over the long term for some, and possibly many people (even if it does help their blood sugar and insulin regulation). For many others, it seems that high fat does a lot of good for them. And good for them. They have found what works for them.
Denise, your comments in this thread honestly sound more like wishful thinking than like logical analysis.
For example, with respect to the Esselstyn study, the "nonadherers" are nothing like a control group. In a modern, well designed study, the "nonadherers" would be included in the experimental group based on intention to treat. So what happens if you add the "nonadherers" back into the stats for the diet? Doesn't look so good any more, does it? Worse than Nielsen and Joensson, perhaps?
Nor was Esselstyn treating what would be considered a particularly high risk group today. Most men over 50 today would be in that group. Not too many are at a BMI of 36 yet, though.
I don't see how you can argue that very low fat could potentially cure diabetes rather than just put it in remission - that is, allow diabetics to return safely to a Standard American Diet of potato chips and soda pop - and at the same time defend the Barnard study's late degradation of results based on the patients having departed from very low fat after 22 weeks.
It's notable that Swank, whose data are the only older data you present that are rigorous enough to have more than suggestive value, kept his patients on his diet for a lifetime.
Peter, interesting if technical post as usual. After going through the comments, I need to reread it to understand it better.
However, I am a bit puzzled about the reference to fructose, unless you are specifically discussing hepatic tissue. The hepatic portal ensures that the liver has a chance to remove about 99.9% of fructose before it has a chance to reach the rest of the body. It's possible that the liver could be overburdened and fructose concentrations could break through with some modern foods - dissolved liquid sugars, perhaps? - but it's hard to imagine with any foods we're remotely adapted to, such as fruit or, likely, starch or even solid sugar.
@George "Because it is hard....( to eat low fat)"
I completely agree. Many years of struggling to eliminate fat and salt and etc from my diet just made the biomarkers worse, much worse. I then had a terrible g.i. infection that lasted for weeks and when I eventually could eat again I subsisted on plain potatoes. 'Anhedonic' truly describes this diet but bleak would be a better word. After three days of it I couldn't keep away from real food. I could no longer resist butter & cheese. OTOH eliminating wheat beans rice etc has been so easy that I hardly even noticed.
To add to your two clear choices, if living on a mixed diet ie Denise's 'swamp' where most people would find themselves, it is far healthier to progress to eating fewer carbs than it is to eating less fat without going all the way to either extreme.
C.
Imagine two people with type 2 diabetes.
Person A has a lot of insulin resistance, but his pancreas is still able to produce insulin, just not enough to cover the insulin resistance.
Person B's pancreas is worn out and simply can't produce much insulin even though she doesn't have much insulin resistance.
Put them both on a low-fat, high-carb diet that reduces their insulin resistance.
Person A is now able to cover the carbs, and has better blood sugar levels. Person A gets better.
Person B can't produce enough insulin even on a standard diet, but her pancreas is even more challenged on the low-fat, high-carb diet, and Person B gets worse.
There would also be some between these extremes, and they would see no change.
This is one reason studies of "diabetics" are so difficult to interpret. In the early days, they didn't even distinguish between type 1 and type 2, and those studies are pretty meaningless.
That totally makes sense Gretchen.
Before insulin it was easy to tell who still made it as only people with little or no insulin were diagnosed, because glycosuria and ketonuria were the diagnostic signs. In practical prognostic terms there wasn't much difference between these type 1 and late-stage type 2 cases, except that the most definite type 1 cases were the children so growth was an extra problem.
They both stayed alive on a high fat low carb diet with limited protein and ample calories, at least in the short-to-medium term (2 or 3 years) that there's good data for (discovery of insulin limits the period for observation) and this was preferable to a starvation diet. Occasionally a type 2 recovered on this regime, which was probably pretty terrible nutritionally compared to today's low carb diets, plus they had no glucose or ketone monitors of any kind except urine tests.
https://www.dropbox.com/s/zpwhed7aw7lwk2o/Newburgh-1923-%E2%80%9CFurther%20Observations%20on%20the%20Use%20of%20a%20High%20Fat%20Diet%20in%20the%20Treatment%20of%20Diabetes%20Mellitus%E2%80%9D.pdf?dl=0
Wishful thinking is about right.
I would also classify low-fat into 2 groups: the high grain consumers and the Michael Pollan's 'Eat food, not too much, mostly plant' type.
Clearly the latter group is metabolizing fat from gut bacteria and calorie-restricted.
I'm not hopeful for the former group.
Chacun a son gout.
Hmm, or oppositely, put both on a very low carb diet diet and the insulin resistance is almost irrelevant. If sufficient weight is lost on this regime that will also fix the insulin resistance in Person A. It seems to me that there is more advantage in this plan.
There is also more than one type and/or locale of insulin resistance.
C.
@George. Pre-insulin it was easy to tell a type 1 from a type 2 because the type 1s all died. The disease was 100% fatal.
Type 2s will also spill glucose if their blood sugar gets too high. I'm type 2, and when I was Dx'd, my urine was so high in glucose they tested their machine to make sure it wasn't broken. In early days, they considered the disease well controlled if the patient wasn't spilling glucose. But those levels (below 180 mg/dL for most people) would be considered too high today.
The difference was that type 2 don't normally secrete ketones. But there are always exceptions, and there is a type of diabetes called "ketosis-prone diabetes" or "Flatbush diabetes" that has some characteristics of type 2 and some of type 1.
@Gretchen,
read the link I posted. Mortality of type 1s was high but short-to-medium term mortality could be controlled - no deaths of children in 3 years on their diet. No DKA. Type 2s were dying too.
Flatbush diabetes is very interesting.
"Mortality of type 1s was high"
Like 100%. No mother would watch her child starve to death if the child could live. Even starvation only extended life for a few years, and one wonders if that life was worth living. See photo at http://www.diapedia.org/type-1-diabetes-mellitus/natural-history.
Three years is better than no years, but diabetes was still a death sentence.
If some survived for years, they were probably type 2 (which hadn't been discovered yet) or MODY or something else.
@Gretchen "Put them both on a low-fat, high-carb diet that reduces their insulin resistance."
perhaps some problems with this assertion? Unless it is super-duper-ultra low fat I don't think there is much validity in it. Otherwise it is the same-old modern Cant such as we hear from the various diabetics associations and Prof B-M. OTOH it seems very clear and quite well supported by various studies that there is an almost linear dose-dependant cluster of benefits from reducing dietary carb, even if you don't reduce it entirely.
C.
@passthecream. Yes, I meant superduper ultra low fat. See the last graph in this blogpost.
http://www.healthcentral.com/diabetes/c/5068/163018/diets-bg-levels
That woman is not diabetic, but some people with diabetes may also see improved BG levels on a low-fat diet. I myself do much better on a low-carb diet, but I can accept that not everyone is like me.
@Gretchen,
the children that Joslin treated were horribly starved, but those treated by Newburgh and Marsh were not, the calorie ration is fairly high by today's standard. Certainly no mother would want their child on such a restricted diet, but that is not the point. Insulin was not available. Elliot Joslin had been extending life with starvation since before the First World War, as described here.
You often see the claim online, for example in the Joslin Diabetes Centre's own website, that "before insulin, the only treatment was a “starvation diet”", but this is because the work of Newburgh and Marsh, being later and overtaken by the discovery of insulin, is not as well known. It seems likely that had insulin not been discovered and mass produced, the high fat diet would have replaced the starvation diet eventually.
The Starvation diet paper claims (in 1915)
It will be noticed that the diets which follow contain rather small amounts of fat, a good deal less than is usually given to diabetics. There are two reasons for this: In the first place, we do not want our diabetics, our adults, at any rate, to gain weight; and in the second place acidosis is much easier to get rid of if the fat intake is kept low.
http://www.gutenberg.org/files/26058/26058-h/26058-h.htm
(Note that only the adults can gain weight - the kids are type 1.)
In 1923 Newburgh and Marsh are saying the opposite, that the high fat diet is preventing DKA.
"Not only does acidosis not develop in patients who are living on this diet, but it is a fact that all our patients showing at admission an acidosis short of coma rather promptly lost their acidosis while taking the high fat diet."
They compare their results (in a hospital that took in emergency and charity cases, often with complex problems on admission) with Joslin's (in a private clinic purely for the treatment of diabetes) and find them comparable.
At the exact same time Karl Petren, who ran a clinic in Sweden, published a report that high fat feeding prevented ketonuria in his patients.
"if the fat content of the diet is sufficiently great and if the protein content is restricted, the ketosis of diabetes can be abolished"
Why the difference? Perhaps because Joslin was working his patients' carb intakes back up to their tolerance level, while Newburgh and Marsh had a set level (<35g) and preferred to increase fat.
The thing is, the question was never answered, the high fat diet (but not the starvation diet) was forgotten, and all we have is the clues from Newburgh and Marsh's 3 papers, a paper by Karl Petren in German (but cited in Nature in the 1950's), and the work on alloxan-treated dogs and various other animal models of T1D, where feeding fat, e.g.
"1939. Marks and Young demonstrate that when dogs made diabetic by daily injections of anterior pituitary extract are given a diet which is almost exclusively fat the glycosuria and ketonuria of diabetes are greatly diminished. “It seems as if on a fat diet the metabolism of these dogs ceases to be abnormal.”
It's still a mystery why this is.
George, alloxan sounds like nasty stuff.
There's an interesting symmetry here; that zero fat input disables insulin production and zero carb input disables glucagon production, due to small amounts of those substrates being involved in the triggering of those two hormones respectively ie fat for insulin and glucose for glucagon.
Gretchen, for me also LC is the only solution that works, effortlessly. I have normal pp BG of around 5.5 nowadays. 10 years ago it was 17mmol/l (310 in your units). As you would know it doesn't only go out with urine also taking many nutrients with it, it also seeps out of your skin causing infections and rashes, wrecks connective tissues, weakens keratin, hardens crystallin etc; it pickles you from the inside out.
C.
@George. It was Allen, not Joslin, who promoted the "starvation diet" at his Allen Institute. The father of a friend was there just before the discovery of insulin. He was 12 and weighed 45 pounds and wrote home in delight when they allowed him an extra cube of cheese. He was determined to survive until a cure was found, and he did.
One problem with interpreting early studies is that you don't know if they were type 1 or type 2 or something else. People have been arguing about diabetic diets for eons, and they've ranged from feeding diabetics candy because they were losing sugar in the urine to the Rollo diet of blood pudding and old rancid meat. Some of them helped some patients, but none kept type 1 children alive for long.
If Newburgh and Marsh's diet had kept type 1 children alive for years and years, I'm sure it would have been adopted.
But this isn't the place to discuss historical diets. Peter is trying to explain the mechanism of "carbosis," which does seem to work in some subsets of people with diabetes.
Hi @Gretchen,
The limitation on protein in pre-insulin diets must have been unendurable. The instruction to boil veges 3 or 4 times shows that these must have nutritionally dire diets (as there's not a lot of micronutrition or electrolytes in fats). It seems like the only thing they got enough of was carotene.
Newburgh and Marsh's, and Petren's, papers were published in 1923 by which time insulin mass production (1922) was a reality, and of course the doctors with big diabetes case loads were the first to be given access to insulin. So insulin was naturally adopted before the starvation vs fat comparison really started. The high fat and starvation diets weren't preventing damage and eventual mortality from glycation, cases still had to endure hyperglycaemia, obviously insulin was needed, but the important point is that DKA could be stopped without insulin by LCHF diets and could be rapidly triggered by patients eating high carbohydrate low fat (as shown by Wilder's experiments).
This is relevant because if we hypothesise that very low fat (carbosis) and very low carb (ketosis) are equally good for type 2, yet only one of these options would be at all tolerable to an untreated type 1 case, or indeed to an end-stage type 2 case, then I think the hypothesis falters in its pragmatic implications, because this predicts that ketosis will have a superior safety. As seen by the 15% getting worse on the rice diet.
The Newburgh and Marsh paper compares results with those of Joslin's clinic because Joslin published relevant results, though the theory of "eating to the capacity of the pancreas" was Allen's, and Elizabeth Hughes Gossett, the first person to be given insulin in the US, was Allen's patient. George Graham in the UK was another who had some success with a modified starvation diet. There are two unusual cases here and they seem to have had characteristic bone growth of type 1.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2153338/pdf/procrsmed01414-0024.pdf
Let's assume that the 4 year survival in that paper is a prolonged honeymoon period - as Allen would have predicted, it is the avoidance of carbohydrate that has extended it.
Whether a very low fat diet is safe in diabetes depends on the condition of the pancreas. There are going to be diabetic states where it is either immediately unsafe or will promote progression. This seems to be less true of a very low carb diet.
@George, your points are very well made I think,
and " ... predicts that ketosis will have a superior safety."
Leads me to mention something a bit tangential but with interesting connections. You might have noticed in the popular press recently, big excitement over the potential of nicotinamide to lower the risk of certain types of skin cancers.
That reminded me that there is a relation between some ketones and B3 derivatives in that they target similar receptors. Which then prompted me to re-visit Thomas Seyfried's talks and dig out the reference to ketones as natural Histone Deacetylase Inhibitors. Nicotinamide together with other nadh derivatives are one class of HDI's. It's a roundabout trail but it leads to this type of work:
http://www.ncbi.nlm.nih.gov/pubmed/23223453
Bringing this back to the current discussion, I don't think you would have any chance of developing high levels of ketones on a total carbohydrate diet with normal metabolism so it could be anti-therapeutic in that sense.
C.
I remember Steve Phinney talking about histone deacetylase inhibition by ketone bodies when I heard him speak in Auckland last year.
So therapeutic effects of ketones, and ketone protection of brain function during hypoglycaemia, are two things we risk losing if we assume ketosis and carbosis are equivalent.
Although carbosis could be targeted at specific T2D cases who would benefit more than from LCHF, based on genetic testing or high tech diagnostics available in some places for a price, most people in the world don't have this luxury. There are also places in the world where insulin is unavailable, and others where it is irregularly available or people do not earn enough to pay for it.
For this reason the default diet for diabetes should be set as the one that works best when diagnostics are primitive and insulin may not be available.
Very Low Fat Experiment: Conclusion by stevecooksey
Hi all, half term here, will get to comments as soon as practical!
Peter
What about soft drink ketosis?
That's a carbosis and a ketosis rolled into one.
Awesome. Thanks P.
Consider too, the effects of a carbosis diet vs. ketosis diet on oral health.
That can't be a small difference there, long term.
Also, are/would successful carbotic dieters be a slave to snacking every couple of hours?
KT
Ah, this is a quote from Denise M., from an interview at another site before the current post on Carbosis:
"I was seventeen. It’d been a full year since I’d become a strict, low-fat, fruit-noshing raw vegan — led there by a cocktail of food allergies and dewy-eyed trust in people from the internet (bad idea is bad). Perhaps too distracted by my constant brain fog, perpetual shivering, and the clumps of hair making a mass exodus from my scalp, I’d failed to notice the prime victim of my lopsided diet: my teeth."
?
C.
Re: oral health: Denise has written on her blog elsewhere that she eats several solid meals a day, rather than grazing, and takes specific supplements for better dental hygiene (cod liver oil and vit k2, IIRC).
Chacun a son gout I suppose. I don't understand the difference between 'several solid meals'; and grazing. Maybe it would be healthier to have two or three meals of more satisfying food and no need for supplements.
C.
Grazing, low fat for diabetes -
It all seems to be based on the Staub-Traugott effect
https://en.wikipedia.org/wiki/Staub-Traugott_Phenomenon
The Staub-Traugott Phenomenon (or Staub-Traugott Effect) is the premise that a normal subject fed glucose will rapidly return to normal levels of blood glucose after an initial spike, and will see improved reaction to subsequent glucose feedings.
This can also apply to compensated type 2 diabetes. But it's about pure glucose over a day or so - not a meal, and certainly not a series of meals and snacks for years and years.
I think this premise partly underlies high-carb recommendations for T2D.
There is a mention of early VLF diets here, in Woodyatt's brilliant 1921 vindication of Newburgh and Marsh's high fat diet for diabetes.
https://www.dropbox.com/s/500oew1a48a4uwa/woodyatt1921.pdf?dl=0
Woodyatt can't explain the rice diet effect, but he does acknowledge it.
This study appears to be supportive of the hypothesis presented.
http://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-015-0038-x
@ erdoke,
if they had a theory about saturated fat in that context, they should have tested it with a coconut oil arm, like these guys
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1805500/
or these guys
http://www.ncbi.nlm.nih.gov/pubmed/26200659
New article that mentions carbosis diets:
http://www.womenshealthmag.com/food/side-effects-of-vegetarianism
High glucose + high FFA = oxidative stress. Another supporting paper?
Tabara et al.: Synergistic association of elevated serum free fatty acid and glucose levels with large arterial stiffness in a general population: The Nagahama Study, Metabolism, Volume 65, Issue 1, January 2016, Pages 66-72
http://www.metabolismjournal.com/article/S0026-0495(15)00303-0/fulltext
erdoke, have to be careful with this observational stuff. Elevated FFAs under fasting might be a surrogate for adipocyte insulin resistance. I've not checked my aortic pulse wave velocity recently but when I was 50 I had the value of someone of my height aged 32 years... I'm guessing my FFAs are quite high, all of the time.
Peter
I found a short-term comparison trial/feeding study of ultra low fat (89% CHO, 11% PRO, 0% FAT) vs ultra low carb (89% FAT, 11% PRO, 0% CHO).
Results were not in favour of ultra low fat.
http://www.ncbi.nlm.nih.gov/pubmed/15579777
J Clin Endocrinol Metab. 2004 Dec;89(12):6193-7.
A low-carbohydrate/high-fat diet improves glucoregulation in type 2 diabetes mellitus by reducing postabsorptive glycogenolysis.
Allick G1, Bisschop PH, Ackermans MT, Endert E, Meijer AJ, Kuipers F, Sauerwein HP, Romijn JA.
Author information
Abstract
The aim of this study was to examine the mechanisms by which dietary carbohydrate and fat modulate fasting glycemia. We compared the effects of an eucaloric high-carbohydrate (89% carbohydrate) and high-fat (89% fat) diet on fasting glucose metabolism and insulin sensitivity in seven obese patients with type 2 diabetes using stable isotopes and euglycemic hyperinsulinemic clamps. At basal insulin levels glucose concentrations were 148 +/- 11 and 123 +/- 11 mg/dl (8.2 +/- 0.6 and 6.8 +/- 0.6 mmol/liter) on the high-carbohydrate and high-fat diet, respectively (P < 0.001), with insulin concentrations of 12 +/- 2 and 10 +/- 1 microIU/ml (82 +/- 11 and 66 +/- 10 pmol/liter) (P = 0.08). Glucose production was higher on the high-carbohydrate diet (1.88 +/- 0.06 vs. 1.55 +/- 0.05 mg/kg.min (10.44 +/- 0.33 vs. 8.61 +/- 0.28 micromol/kg.min) (P < 0.001) because of higher glycogenolysis. Gluconeogenic rates were not different between the diets. During the use of hyperinsulinemic euglycemic clamps, insulin-mediated suppression of glucose production and stimulation of glucose disposal were not different between the diets. Free fatty concentrations were suppressed by 89 and 62% (P < 0.0001) on the high-carbohydrate and high-fat diet, respectively. We conclude that short-term variations in dietary carbohydrate to fat ratios affect basal glucose metabolism in people with type 2 diabetes merely through modulation of the rate of glycogenolysis, without affecting insulin sensitivity of glucose metabolism.
There's also this one in healthy men - again, high fat (83%) favoured glycogen storage of glucose.
http://ajcn.nutrition.org/content/73/3/554.long
Dietary fat content alters insulin-mediated glucose metabolism in healthy men
Results: During hyperinsulinemia, endogenous glucose production was higher after the HFLC diet (2.5 ± 0.3 μmol•kg−1•min−1; P < 0.05) than after the IFIC and LFHC diets (1.7 ± 0.3 and 1.2 ± 0.4 μmol•kg−1•min−1, respectively). The ratio of dietary fat to carbohydrate had no unequivocal effects on insulin-stimulated glucose uptake. In contrast, insulin-stimulated, nonoxidative glucose disposal tended to increase in relation to an increase in the ratio of fat to carbohydrate, from 14.8 ± 5.1 to 20.6 ± 1.9 to 26.2 ± 2.9 μmol•kg−1•min−1 (P < 0.074 between the 3 diets). Insulin-stimulated glucose oxidation was significantly lower after the HFLC diet than after the IFIC and LFHC diets: 1.7 ± 0.8 compared with 13.4 ± 2.1 and 19.0 ± 2.1 μmol•kg−1•min−1, respectively (P < 0.05). During the clamp study, plasma fatty acid concentrations were higher after the HFLC diet than after the IFIC and LFHC diets: 0.22 ± 0.02 compared with 0.07 ± 0.01 and 0.05 ± 0.01 mmol/L, respectively (P < 0.05).
Conclusion: A high-fat, low-carbohydrate intake reduces the ability of insulin to suppress endogenous glucose production and alters the relation between oxidative and nonoxidative glucose disposal in a way that favors storage of glucose.
Full-text of ultra low fat vs ultra low carb (14 days on each diet, cross-over design, n=7)
https://www.dropbox.com/s/ug8ahcsgf5nfagg/Allik%20HF%20vs%20HC%202004.pdf?dl=0
Thanks George,
I have an impression that my glucose level during a day long fast is lower if the fast is orally fat supplemented. Sipping cream on occasions will often have BG in the 3.5mmol/l region compared to over 4.0mmol/l on a water (black tea) fast. Interesting, I think you have written about fatty acids lowering blood glucose...
Peter
If anecdotal evidence is worth anything, this stuff definitely bears out for me. If I have a carb binge day, I literally have to wait until the carbs have left my digestive tract completely before I eat cream/chocolate, or I will trigger some serious asthma and inflammation symptoms, and this happens pretty much instantaneously. Take a bite of chocolate, can't breathe. When I am low carb, I can drink as much cream as I want and I may as well be drinking water for all the inflammation it causes.
On the other hand, I can eat all the shitty chinese takeout I want, no matter how much PUFA they fry it in, and not have anywhere near the same inflammatory symptoms. However, the PUFA will trigger what feels like very mild neuropathy after a short time, and some other very weird symtpoms that I'm pretty sure aren't good.
Maybe the association of the mediterranean diet with longevity has something to do with the balance they strike by combining carbs with olive oil. Perhaps the high saturated fat diet is healthiest when carb intake is kept very low, but as soon as carbs are introduced it seems like inflammation becomes a major issue. By replacing SFA with MUFA, you get the best of both worlds. You get the benefits of a high fat diet combined with not having to continuously worry about restricting carbs.
Coincidentally Rattus as it happens I have just written a post about a new complex and expensive study designed to not shed light on that very question
http://hopefulgeranium.blogspot.co.nz/2016/03/the-state-of-nutritional-science-2016.html
Thanks for the link George.
For me personally, the high sfa - low carb diet is far superior performance-wise to the mufa-carb diet. Being realistic though, probably the only people who will ever restrict carbs enough to benefit from a high SFA diet are the ones who are forced to by their broken metabolisms. For everyone else, a carb-mufa balanced diet would probably be much easier to adhere to, and is at least a significant improvement over the SAD.
Even so, Rattus, there are exceptions -
Gestational Diabetes is a state in which insulin resistance is natural, but is over-loaded by the anti-insulin hormones of pregnancy in those at risk of type 2 diabetes.
In this condition SFA (butter) with a meal (bread and low-fat cottage cheese) improves glycaemia more than MUFA (olive oil) does.
"The area under the curve showed a significantly lower glucose concentration for SF meal (p = 0.001). Serum insulin concentrations followed the glucose response with the peak at the 60-min time point and a significantly lower concentration at the 180-min time point in the SF than in the MUFA group. The present study demonstrated that the addition of SF to the meal resulted in lower postprandial glucose and insulin than when the meal contained MUFA. Thus, SF may be useful in controlling postprandial glucose."
http://www.ncbi.nlm.nih.gov/pubmed/10774766
Sure, same would be true of a fat person. The more insulin resistant you are, the more SFA is going to work well for you. In my experience tho, the more insulin resistant you are, the more those carbs will cause inflam., so maybe the pregnant lady should eat just the butter. For everyone else, the goal should be to AVOID insulin resistance.
Good article. When dealing with peole with diabtes (as a practiitoner), I wonder if there is a way to determine ahead of time whether a diabetic will fall into the 63% category and do well on carbosis or whether a lower carnb diet of 130g will serve hom/her beter. Also 130g carbs is only about 520 calories, seems like most of the rest of the calories may require mostly MUFAs.
Hi E Klein,
Why should anyone want to go to carbosis? What's wrong with a fatty steak and some broccoli with plenty of butter?
This is what puzzles me. White rice and sucrose (for carbosis) may be someone's preferred diet, or it may not. No thanks...
Peter
Hi E,
From the literature it looks as if 70g/carb/day is the cut-off for really marked benefit in diabetes, as for the MUFA question, you want to be burning depot body fat, and the metabolism self-corrects when fasting on this mix - depot body fat (if we go back to before the seed-oil craze) is about 60% MUFA, 30% SFA, and 10% a mix of PUFA and MCFAs.
That's like a mix of butter and olive oil, with a little coconut oil thrown in.
@E Klein ND,
A group of diabetics in UK joined forces to run a blog about benefits of low-carbohydrates diet particularly for the people with diabetes.
http://thelowcarbdiabetic.blogspot.com/2016/09/diets-higher-in-animal-and-plant.html.
You may also check the blog of a registered dietitian from US Franziska Spritzler, RD, CDE http://www.lowcarbdietitian.com/blog.
Fascinating topic, thank you. Here are some related historical studies beyond the Kempner rice diet: https://www.youtube.com/watch?v=5xa1b-15H5g
Where does this leave people who are not T2 Diabetics ?. Does anyone have links to long term data/studies on LCHF diets on people who start out 'healthy'. What about the argument, which seems to be endorsed in this report, that we are asking the wrong question. Should we be asking what diet is best for any individual.
Rice is not the only way to go carbosis! You can freely eat fruits, tubers, vegetables and legumes except soy! It can be a delicious way to eat! I have been practicing it <10% fat for 3 years with excellent results
Rice is not the only way to go carbosis! You can freely eat fruits, tubers, vegetables and legumes except soy! It can be a delicious way to eat! I have been practicing it <10% fat for 3 years with excellent results
Hi adam, sorry for the delay.
I'd view it slightly differently. Saturated fats would simply signal satiety sooner than MUFA. End result would be eating less and eating less would induce lower insulin. MUFA would allow more fat storage before satiety but would generate less insulin initially. I think it would pan out pretty evenly on a mixed real food diet. Once you add sucrose the system falls to pieces. Sucrose above a threshold generates insulin resistance per se. Adding saturated fat to that is not a good idea. But no one should blame butter for what the jam did...
Peter
Hi Peter, would you like to know your opinion about which kind of food approach is most suitable for a person trying to build muscles? Does it make sense for a short time to stay low in fat? what do you think of the "body-recomp? is it really possible? thanks for the excellent work you do!
Hi Peter, would you like to know your opinion about which kind of food approach is most suitable for a person trying to build muscles? Does it make sense for a short time to stay low in fat? what do you think of the "body-recomp? is it really possible? thanks for the excellent work you do!
Interesting that some people respond to low fat, while others respond to low carb. Couldn't it be that this is genetically dictated? Somewhere along the line humans evolved in varying locales w varying availability of macro-nutrients. Some genotypes became better at carb metabolism, others at fat metabolism. Minger even invokes Pritikins ancestral hypothesis w high carb eating cultures, whereas Paleo/Primal advocates does the same w high fat cultures.
Cardiologist Tom Dayspring alludes to this (featured in this post) suggesting about one third of patients don't do well on high fat diets with regard to LDL levels. https://bjjcaveman.com/2014/11/17/ketosis-and-high-cholesterol-according-dr-thomas-dayspring/
Also, as highlighted in this podcast by Rhonda Patrick, the FTO, PPAR-alpha and PPAR-gamma genes, regulate how individuals metabolize saturated fat.
I think Dayspring's clinical findings and Patrick's research findings are probably two sides of the same coin. https://podcastnotes.org/2018/03/27/the-art-of-manliness-dr-rhonda-patrick-on-how-to-optimize-your-body-with-micronutrients-genetic-nutrition-and-intentional-stress/
So it may be possible, with genetic testing of these genes, or LDL response to saturated fat, to identify who may benefit from high carb instead of high fat and vice versa. Then we don't need to gather in one camp or another pointing fingers, its truly individual.
My guess is that Peters LDL doesn't go to 200 when he eats butter, that his FTO and PPAR genes allow a higher fat content in his diet without adverse effect. And that he would change his tune quickly if butter was clearly putting him at higher risk of atherosclerosis as Dayspring describes.
Yes you can do higher MUFA instead of SAFA, but gone are the butter and steaks and you're eating nothing but macadamia nuts and avocado all day. Not much better than fruit and veggies all day.
Post a Comment